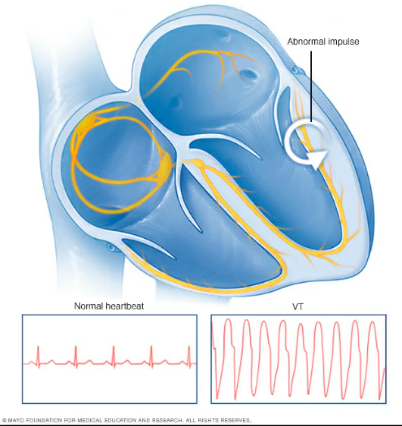
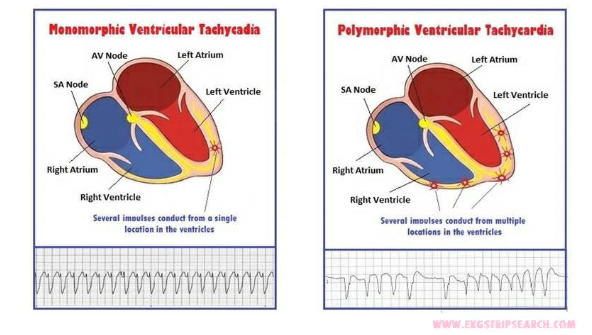
The heart has two upper chambers, which are called atria, and two lower chambers, which are called ventricles. In normal rhythm, the heartbeat starts in the sinoatrial (SA) node, which acts as the heart’s natural pacemaker in the upper right chamber. The SA node sends an electrical signal to contract the atria. The signal then moves throughout the heart’s electrical system, which causes the ventricles to contract. In ventricular tachycardia, the electrical signal starts at a site in the lower chambers of the heart.
Symptoms may start and stop suddenly. Brief episodes of ventricular tachycardia may not cause any symptoms in some people. Others may experience:
Sustained or more serious episodes of ventricular tachycardia may cause:
Any condition that puts a strain on the heart or damages heart tissue can increase your risk of ventricular tachycardia. Lifestyle changes or medical treatment may decrease the risk associated with the following factors:
The most effective way to prevent ventricular tachycardia is to reduce your risk of developing heart disease. If you already have heart disease, it is important to monitor your heart disease and follow your treatment plan to lower your risk of ventricular tachycardia.
Once you have been diagnosed with VT, you will likely be asked to undergo testing to evaluate for underlying causes. Workup may include one or some of the following:
Based on the type of ventricular tachycardia that you have (sustained or nonsustained), what the morphology (form) of your VT is, and whether you have structural heart disease will determine what type of treatment your provider will recommend to you.
Treatment options may include one or a combination of the following:
There are 3 treatment options for VT in patients with structural heart disease, although many patients require a combination: an ICD, antiarrhythmic medications, or catheter ablation.
Many patients at risk for VT with structurally normal hearts are at risk of sudden cardiac death and, as such, are treated with an ICD.
Antiarrhythmic medications that modify the conduction of the electric impulse of the heart can be effective in suppressing VT.
There are two main treatment options for VT in patients without structural heart disease: medications or catheter ablation.